Loneliness is currently a key concern for policymakers, researchers and practitioners across health and social care. Several initiatives have been recently established to address this. One of these, which brings together researchers from different disciplines to
Loneliness is currently a key concern for policymakers, researchers and practitioners across health and social care.
Several initiatives have been recently established to address this. One of these, which brings together researchers from different disciplines to address loneliness, was launched today. The Loneliness and Social Isolation in Mental Health Network aims to foster innovative and boundary-spanning research in order to answer some pressing questions.
This is important work. Loneliness can be a distressing experience and it shortens lives.
I am also concerned how being alone has become a social problem. People with small social networks have become pathologized, a ‘problem’ which needs to be solved. However, it is not always within individuals themselves where the problems lie, but in our society. The elevated position of individualism has downplayed the importance of families and communities, leading to a decline in connectivity.
This is somewhat ironic at a time when social media is so prominent in many people’s lives. But the kind of social connections required are those which involve the exchange of resources which bring mutual benefit, rather than online spaces in which people clamour to be heard.
Social workers have a role to play in enhancing the connectivity of people with mental health problems. This both helps to address the inequality in access to social capital which they face, and to reduce loneliness. To support this, as academic lead of the Think Ahead training programme for mental health social workers I have trained three cohorts how to use Connecting People in their practice.
Connecting People
Connecting People is an evidence-informed approach to supporting people to connect with others. It was developed from a study of how health and social care workers support people with mental health problems to develop and mobilise social capital. This, and subsequent Connecting People research in England, was funded by the NIHR School for Social Care Research.
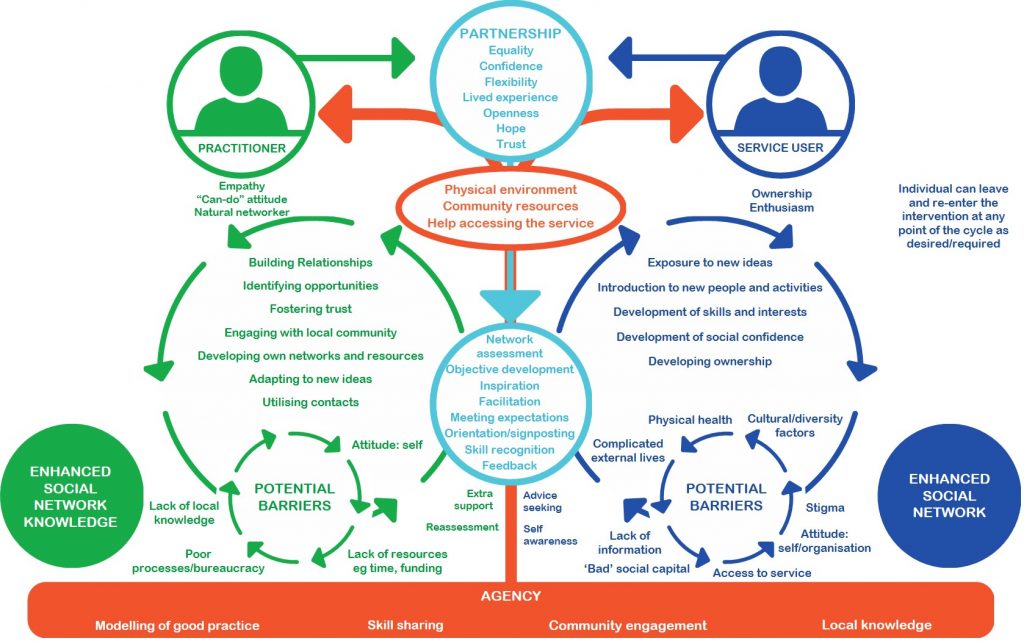
The Connecting People model articulates the processes involved with practitioners and service users working together to increase their social connections, and the barriers both may face. Unlike many social interventions, it integrates a role for the practitioner’s team or organisation within the model.
Teams which are more embedded within the communities in which they work are more effective at enhancing service users’ social connections. This was the primary finding of a large pilot of Connecting People in a range of voluntary and statutory sector teams. However, we found that Connecting People was only fully implemented in one of the community mental health teams in the study.
So, we drew upon participants and graduates of the Think Ahead programme, and Consultant Social Workers who supported their practice learning during their training, to help us evaluate the extent to which they could implement Connecting People in community mental health teams in Durham, Bradford, Essex, Hertfordshire and North Somerset. Working with practitioners and service users, we developed an implementation toolkit, comprising guidance on training, practice and implementation.
“I wanted to be involved in the implementation study as I truly believe that social approaches to mental health can enhance recovery beyond the traditional mental health treatment pathways,” said Simon Owens, Consultant Social Worker at Durham County Council.
“Being able to support our service users to connect to systems, building meaningful relationships and thus develop social capital can provide a longer lasting and positive impact for them. Improving outcomes around wellbeing, mortality and happiness is equally as important as helping someone access medication and therapy for severe and enduring mental health problems.”
“As an integrated mental health service, we recognise the importance of applying both medical and social models with our service users. Providing the initial stabilisation and intervention that people require, whilst also recognising that developing systems, networks and social capital strengthens people’s resilience, may provide them with the self-sufficient support that can prevent them from revolving through services. We need to work smarter, innovatively and put our service users at the centre of what we do. That is why we want to be part of Connecting People.”
The Connecting People Implementation Study, conducted in collaboration with the University of Central Lancashire, London School of Economics and Political Science and the McPin Foundation, has recruited over 150 service users from implementation and control teams (the latter do not have access to the implementation toolkit). They are currently being interviewed for a second time to evaluate the impact of the implementation of Connecting People on their health and social care outcomes. A process evaluation is also underway to understand more about how teams utilise the practice model and the barriers to its full implementation. I will report the findings of this study on this blog in April 2019.
A policy priority
Community mental health policy is gradually becoming more oriented towards the communities in which teams are located. If models such as Connecting People are implemented fully, this will help achieve this policy goal.
Some positive steps towards this goal have already been taken. For example, an injection of £4.5m funding for social prescribing projects across England was announced by the government in July. Connecting People is a step-up from social prescribing, which typically only signposts people to voluntary sector services, but this funding boost is most welcome.
Promoting active and supportive communities is one of six themes of Making it Real, Think Local Act Personal’s guidance on personalised care and support. Connecting People is one way to make this happen.
Connecting People is a strengths-based approach to engaging people with communities. It is cited in Social Work for Better Mental Health as a way for mental health social workers to fulfil one of their key roles. But it is becoming increasingly apparent that employers – both local authorities and NHS Trusts – need to do more to support social workers to implement it.
This sentiment is echoed by Lyn Romeo in her fourth annual report, which focuses on strengths-based approaches. She argues for greater organisational support for community engagement:
“Social work doesn’t operate in a vacuum. Organisations are important in creating the conditions within which best practice can flourish. … [They] must position professional practice at the heart of the relationship between people, their families and the local community. This includes providing opportunities for practitioners to link up with voluntary agencies and other professionals in the area” (pp. 6-7).
Further information
Connecting People appears to work best where there is organisational support to implement it. If you are interested in finding out more about how your organisation can implement Connecting People, please contact me. Further information about Connecting People, including its adaptation for use in other countries, can be found at https://connectingpeople.net/.
Disclaimer
This blog refers to independent research funded by the NIHR School for Social Care Research. The views expressed are mine and not necessarily those of the NIHR, SSCR, Department of Health or the NHS.
