Mental health social workers make a unique contribution to mental health services. They are respected for their knowledge and application of mental health law, their ability to use psycho-social interventions in complex situations and their
Mental health social workers make a unique contribution to mental health services. They are respected for their knowledge and application of mental health law, their ability to use psycho-social interventions in complex situations and their integration of social perspectives into medically dominated services.
As I have repeatedly highlighted in posts in this blog, mental health social work practice is not underpinned by research to the same extent as in psychiatry or clinical psychology. This is not necessarily a problem. Social work draws on diverse sources of knowledge to understand and work with the messy realities of life. However, when systematic reviews are searched for ‘effective’ interventions which can form the basis of mental health policy, it is rare to find social work practice being articulated.
Systematic reviews rely on evidence produced by randomised controlled trials. These are commonly used to test new drugs or psychological therapies, but are rarely used to evaluate the effectiveness of social work interventions. Quite simply, social work is too complex and multi-faceted to deliver in a standardised way to enable it to be evaluated in a trial. But if that complexity could in some way be articulated in an intervention model and then measured, would it be possible to evaluate it in an experimental study? This is what we are testing in the Connecting People study (funded by the NIHR School for Social Care Research).
Connecting People study
We have taken a routine aspect of social work and social care practice which is insufficiently articulated and evaluated – enhancing individuals’ social connections – and set out to define, measure and evaluate good practice. Social relationships can be important for recovery from mental health problems and social workers can play an important role in supporting people to enhance them.
We began by understanding existing practice. We wanted to find out how practitioners were already supporting people to strengthen existing social relationships and develop new ones. In a diverse set of agencies in the statutory, voluntary and third sectors we talked to over 150 people about their practice and developed a good understanding about what good practice looks like. We articulated this practice and termed it the ‘Connecting People Intervention model’. We wrote practice guidance and training materials to accompany the model and help practitioners understand what it meant for their practice.
In 2012 we took the intervention model, practice guidance and training to 14 diverse teams in NHS mental health services, local authorities and the voluntary sector to evaluate the extent to which their practice is similar to, or different from, the intervention model. We have also been investigating the extent to which the implementation of the intervention model improves outcomes for people who use the services. To do this we have been interviewing people who had recently been referred to each team and we followed them up for a period of nine months. We are now in the process of conducting the final few interviews of this study and analysing data emerging from it. The results will be available later in the spring.
The data from this study will help us to establish if it is possible to conduct an experimental study to evaluate the effectiveness of the Connecting People Intervention. Grounded in the lived experience of practitioners and service users, the intervention model captures practice wisdom which we think helps in the process of connecting people. Arising out of practice, we think the intervention model could be easier to implement in practice. But we are still in the process of finding this out.
Intervention evaluation guidance
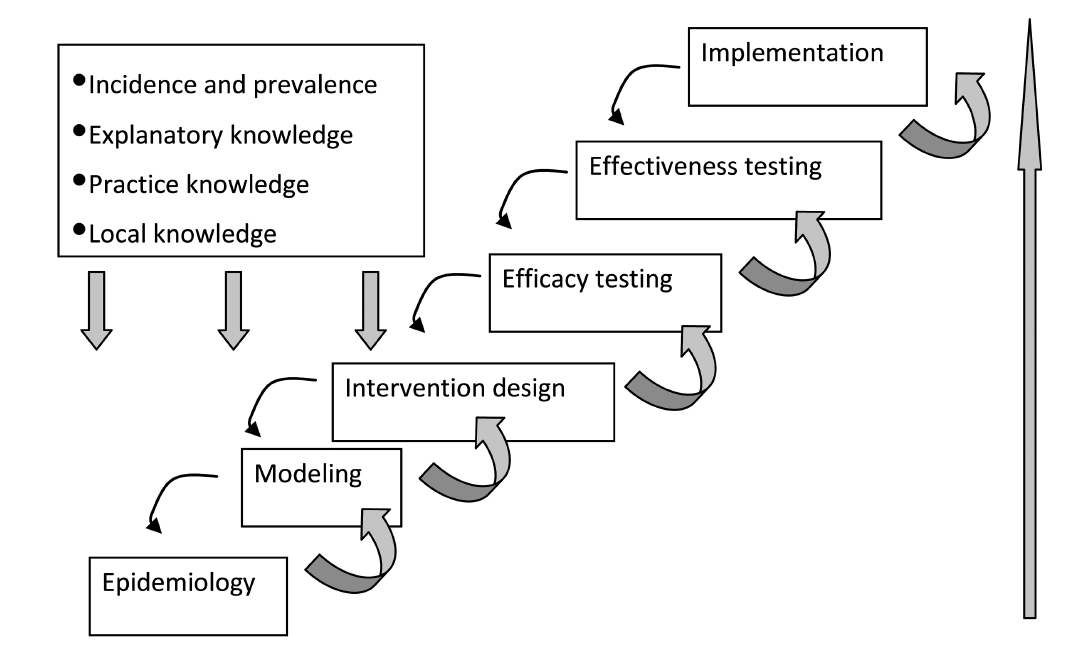
An account of the methodology we have used to develop the Connecting People Intervention has just been published by the Journal of Evidence-Based Social Work. I illustrated the intervention development process using this diagram:
If you are familiar with the Medical Research Council guidance on developing and evaluating complex interventions, you will see some similarities. However, this process emphasises the importance of explanatory, practice and local knowledge at the beginning of the process and feedback loops at each step. Learning from each stage should feed backwards as well as forwards in the process to ensure improvements are made on a continual basis. Also, although ‘implementation’ comes at the end of the process, in reality it is happening throughout. Research and practice are evolving in synergy, both influencing each other.
We hope that our experiences can help other researchers to articulate interventions in such a way that they can become amenable to experimental evaluation. In fields such as mental health social work where evidence of effectiveness is becoming increasingly important, the importance of this process cannot be under-estimated.
More information
The publishers of the Journal of Evidence-Based Social Work have made this paper available free of charge to the first 50 people who click on this hyperlink:
If you are interested in reading the full text of the paper but can’t access it via this link, please contact me and I’ll email you a PDF version of it.



I wonder if your research makes any passing nod to Social Network Theory which was very big when I trained in the early 1970s. Admittedly that was more about bringing the various existing elements of someone’s network together rather than creating new social links, but it did allow for the expansion of those networks. Quite a lot of Personalisation is aimed at helping the individual to articulate their own interests and build social netowrks and contacts around those interests.
Hi Nick.
Indeed it does. Social network theory underpins the research. It’s very much about understanding an individual’s existing social connections and supporting them to develop and maintain relationships which enhance recovery. Networks should not be pathologised. Small is often best. It’s all about what is best for the individual. We’ve a long way to go to bring this work into routine mental health care and support, but we’re working on it!
All the best,
Martin